Kidney disease in Uganda "a community based study "
Abstract Background: Chronic kidney disease (CKD) is a major cause of morbidity and mortality in Sub-Saharan Africa (SSA). The majority of studies on CKD in SSA have been conducted among HIV-infected populations and mainly from large health facilities. We determined the prevalence of CKD and its predictors among populations in communities in central Uganda.
Methods: A cross-sectional study was conducted in Wakiso district using multi-stage sampling. Data was collected on age, sex, socio-economic status, history of alcohol intake, diabetes mellitus, hypertension and smoking. Measurement of blood pressure, weight and height to determine body mass index (BMI) and investigations including HIV testing, fasting blood sugar, creatinine and urinalysis were conducted. Logistic regression was used to estimate the strength of the association between variables and the presence of CKD estimated using the Cockcroft Gault formula.
Results: A total of 955 participants aged 18–87 years were enrolled into the study. The median age was 31 years (Interquartile range 24–42) and majority (67%) were female. Up to 21.4% (204/955) had abnormal renal function with CKD stage 1 in 6.2% (59/955), stage 2 in 12.7% (121/955), stage 3 in 2.4% (23/955), CKD stage 4 in 0% and CKD stage 5 in 0.1% (1/995). Female gender OR 1.8 (95% Confidence Interval [CI] 1.2–2.8), age >30 years OR 2.2(95% CI 1. 2–3.8) and high social economic status OR 2.1 (95% CI 1.3–3.6) were associated with increased risk of CKD while BMI>25Kg/m2 was protective against CKD OR 0.1 (95% CI 0.04–0.2). Traditional risk factors such as HIV-infection, diabetes mellitus, smoking and alcohol intake were not found to be significantly associated with CKD.
Conclusion: We found a high prevalence of kidney disease in central Uganda. Interestingly the traditional risk factors associated with CKD previously documented, were not associated with CKD.
Background :
The global burden of non-communicable diseases (NCDs) continues to increase. The World Health Organization projects that NCDs will account for 46% of mortality in sub-Saharan Africa (SSA) by 2030 [1]. Currently, SSA has a dual burden of both infectious and non-infectious diseases. Chronic kidney disease (CKD) plays a major role as a cause and a consequence of other NCDs. A recent systematic review estimates the current prevalence of CKD in sub-Saharan Africa (SSA) at 13.9%
(95% Confidence Interval [CI] 12.2–15.7) [2]. It is also estimated that by 2030, 70% of worldwide end stage renal disease (ESRD) will be in low income countries like those in SSA [3]. In many countries the majority of CKD-related studies have focused on HIV-infected patients [4]. In Uganda, a plurality of studies conducted in the recent past has focused on HIV-infected patients with little data available on non HIV-infected people [5–9]. This study involved participants with and without HIV in rural and semi-urban communities of Uganda. There are many challenges concerning managing kidney diseases in SSA. First, we currently lack data on the major risk factors for chronic kidney disease in SSA due to lack of renal registries and meticulous longitudinal studies [10, 11]. The second challenge is that the majority of patients have no symptoms in the early stages of kidney disease and only present with advanced disease to health care facilities. In a recent study from a national referral hospital from Uganda, up to 51% (n=111) of patients attending the outpatient nephrology care clinic had ESRD [12]. This is largely because the risk factors that could trigger a high index of suspicion for kidney disease in most of SSA have not been well established [11]. Once a patient develops end stage kidney disease there is need for renal replacement therapy irrespective of the primary cause. Early diagnosis and treatment on the other hand has been shown to delay or even reverse CKD but this is largely driven by screening for known risk factors and treating them [13, 14]. We determined the prevalence for CKD and associated factors in both rural and urban based community settings of Wakiso, Uganda using a cross-sectional design. We also compared the prevalence generated using the different glomerular estimation formulae including the Chronic Kidney Disease -Epidemiology Consortium equation (CKD-Epi), the Cockcroft Gault (CG) and the Modification of Diet in Renal Disease (MDRD) to establish a baseline differences between the formulae.
Methods :
Between August 2012 and August 2013, MEPI-CVD (Medical Education Partnership Initiative on Cardiovascular Diseases) conducted a cross-sectional community based survey in an urban and a rural sub-county in Wakiso district to determine the prevalence and risk
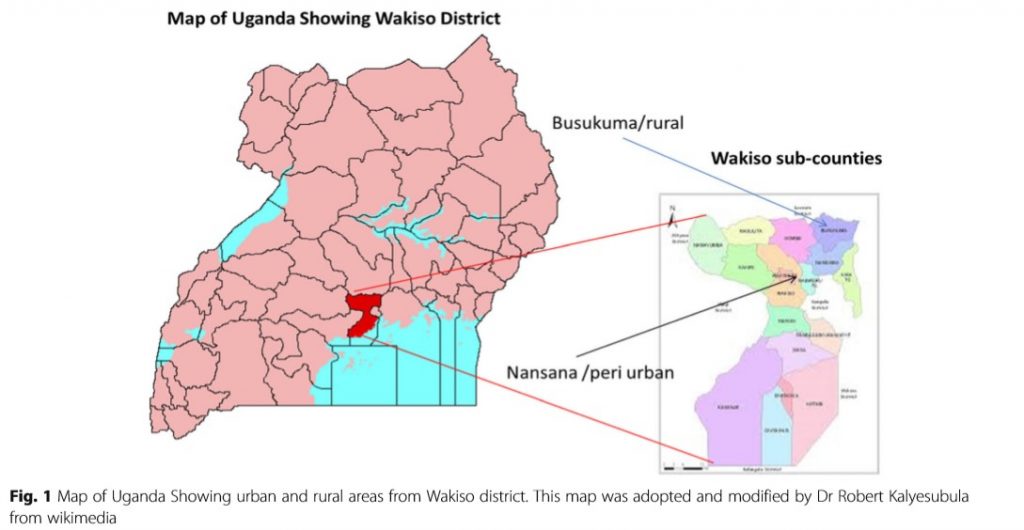
factors for cardiovascular disease [15]. The detailed methods of the MEPI-CVD survey have been described elsewhere [15, 16]. All the sub-counties in Wakiso district were stratified into rural and urban and then one sub-county was chosen from each stratum by simple random sampling. One urban sub-County (Nansana Town Council) was randomly selected out of 5 urban sub-counties and one rural sub-County (Busukuma) was randomly selected out of 13 rural sub-counties in Wakiso district (see Fig. 1. Study Area: Map showing rural area of Busukuma and periurban area of Nansana, Wakiso District, Uganda. Caption: This image was modified from Wikimedia Commons for maps by Dr. Robert Kalyesubula). All households and other key features in the selected sub-counties were mapped and enumerated to generate a sampling frame for the survey. Household locations were mapped using hand-held global positioning system (GPS) receivers. A total of 5,420 households was selected to participate in the survey using a list randomly generated from the household enumeration database. In each of the selected households, one adult (18 years or older) was selected to participate in the survey. Households without an adult were excluded leaving a total of 4,952 participants in the study. Following informed consent, a structured standard questionnaire adopted from WHO STEPS was administered to the household respondents. The questionnaire was administered through face-to-face personal interviews in a research clinic, ensuring a setting that provided maximum privacy to conduct the interview. The data collected included: demographics (age, sex, and address), diet, tobacco and alcohol consumption and medical history, as well as smoke exposure, socio-economic status and family history of NCDs. The researchers also undertook physical measurements for blood pressure, height, weight to obtain the BMI, waist circumference and hip circumference to obtain the waist-hip ratio following standard protocols. Blood samples were obtained via venous phlebotomy for investigations including; HIV, fasting blood sugar and full blood counts. Urine analysis was done using a dipstick. All participants from the primary MEPI-CVD linked study with complete data including urine protein were eligible for the CKD study. During the MEPI-CVD survey, blood samples were stored as plain serum in microvials in a negative 80 °C freezer at the MBN Clinical Laboratory in Kampala, Uganda. The MBN Clinical laboratory is an internationally accredited laboratory with quality standards for both real time and retrospective specimen analysis. We retrieved the stored samples for the randomly selected 1000 participants who met the inclusion criteria and tested their creatinine levels using the Cobas Auto Analyzer (Roche Diagnostics, North America) with a standard reference range of; 66 -106umol/L. Of the 1000 participants 955 had complete samples. The creatinine level measured for each of the participants was used to estimate the glomerular filtration rate using the Cockcroft-Gault formula adjusted for BMI in accordance with previous studies performed in Uganda [6].
Statistical analysis:
To determine the prevalence of kidney disease, we used the proportion of patients with proteinuria of>1+ with an estimated glomerular filtration rate of less than 90mls/ min/1.73 m2 and divided this by the total number of patients recruited in the study. Proteinuria was graded as: negative (less than 10 mg per dL), trace (10 to 20 mg per dL), 1+ (30 mg per dL), 2+ (100 mg per dL), 3+ (300 mg per dL) or 4+ (1,000 mg per dL) [17]. Chronic kidney disease was further staged according severity based on the National Kidney Foundation guidelines [18]. We defined kidney disease as a creatinine clearance of less than 90mls/min/1.73 m2 and chronic kidney disease as a creatinine clearance of less than 60mls/min/1.73 m2. Zscores were generated to compare the proportions at each severity level using the CKD-Epi values as reference [19]. The four categories of the Socio-economic Score (SES) were derived from conducting Principle Component Analysis (PCA) on a statistical software using variables relating to household infrastructure and property ownership. Logistic regression was used to identify factors associated with having kidney disease and odds ratios with their 95% confidence intervals as the measures of association. We adhered to the STROBE guidelines/ methodology for reporting our findings.
Ethics :
Ethical approval was obtained from Makerere University School of Medicine Research and Ethics Committee as well as the Uganda National Council for Science and Technology (UNCST). Patients provided informed consent for the parent study (MEPI-CVD study) and future use of the samples which were stored. Administrative permission to use the stored samples was also obtained from the Principal Investigator of the MEPI-CVD study.
Results Characteristics of participants Of 1000 patients screened from the MEPI-CVD study, 955 (96%) had complete data to determine the prevalence and associated factors for CKD. The remaining 45 participants had incomplete samples for measurement of creatinine but did not differ significantly from those included in the study. We additionally compared the demographics of the 955 participants included for the CKD study with the 3,997 excluded from the original study and found no differences in demographic variables. Of the 955 participants, the majority (67%, n=640) were female and more than two-thirds (73%, n=696) were peri-urban residents. The median age of the participants was 31 years (IQR, 24–42). A total of 93 (9.7%) participants were HIV-infected, while one in four (25%, n=239) were hypertensive-defined as being on drugs for hypertension or having a systolic blood pressure≥ 140 mmHg and/or diastolic blood pressure≥90 mmHg at three consecutive measurements. The majority of participants had never smoked (90%, n=862) nor used alcohol (88%, n=841). A summary of selected characteristics of the participants by gender is presented in Table 1. The rural and peri-urban communities significantly differed on all demographic factors except HIV- infection status and presence of proteinuria. Participants from periurban communities were more likely to be younger, poorer, and normotensive with higher BMI.
Prevalence of kidney disease:
The prevalence of kidney disease in this study population was 15.2% (n=145) using the Cockcroft Gault formula. The prevalence according to CKD stages were; CKD stage 1 in 6.2% (n=59), stage 2 in 12.7% (n=121), stage 3 in 2.4% (n=23), stage 4 in 0% (n=0) and stage 5 (end stage kidney disease) in 0.1% (n=1). A total of 6.2% (59) participants had normal glomerular filtration rates but with urinary abnormalities. More than a fifth (21.4%, n=204) of the participants had renal abnormalities of creatinine and urinalysis detected. Of those with urine abnormalities 3 (0.3%) had proteinuria and 55 (5.6%) participants had hematuria.
.
Diabetes mellitus, smoking and alcohol intake were not key factors associated with kidney disease in this study population, contrary to previous findings. This may be due the fact that the majority of participants did not report use of alcohol or smoking. In a recently completed national survey for diabetes in Uganda, only 1.4% (95% CI 0.9–1.9%, N=3689) participants had diabetes mellitus [36]. The low prevalence of these well known risk factors for CKD in our participants makes any comment of their impact difficult to ascertain. In a study by Stanifer et al., half of the cases of CKD (49.1%) were not associated with any of the measured risk factors of hypertension, diabetes, or HIV-infection [10]. In developed countries and worldwide, the majority of kidney disease is due to diabetes mellitus followed by hypertension [37]. It is thus still unclear as to what may be driving the high levels of kidney disease in the rural and semi-urban areas of SSA. Future research needs to look into the peculiar drivers of CKD in SSA. Hypertension and diabetes mellitus can easily be diagnosed even at the lower facility levels. But if there are other unknown causes such as glomerular (especially post-infectious) and interstitial renal diseases driving the epidemic of kidney disease in Uganda, these need to be urgently identified so that appropriate steps to prevent progression to end-stage renal disease can be effected. Treatment of ESRD is not clinically and economically feasible for most low- and middle-income countries [38]. Our study had several strengths. This was a large community based survey, an attribute that is likely to give a proxy estimate of the burden of kidney disease in Uganda. In addition, our study population was both rural and semi-urban and therefore in a true epidemiological transition. The results of our study can therefore be generalized to many populations on the African continent that are in a similar transition. We also compared the three e-GFR estimation methods and highlighted the significant differences that exist between them which may have far reaching consequences to patient care. However, our study also had a few limitations. The primary study was a survey, cross sectional in nature and some data on key parameters for establishing chronic kidney disease like the abdominal ultrasound scan were missing. We used proteinuria as a surrogate marker well aware that it may be affected by other causes like urinary tract infections among others. Furthermore, proteinuria rather than microalbuminuria was used for this study. In addition, we were also not able to determine whether the kidney dysfunction was acute or chronic because we did not have repeat (>3 month) creatinine. Nevertheless, we believe that this study will create awareness on the magnitude of kidney disease in Uganda and hopefully stimulate further research into the underlying etiology and set in motion ways to prevent it.
Conclusion
We found a high prevalence of kidney disease in Uganda which could not be explained by the traditional causes of CKD and noted significant levels of disagreement in the formulae used to estimate glomerular filtration rates. Further studies are needed to characterize the drivers of kidney disease beyond diabetes and hypertension as the prevalence of these diseases continues to rise.
Abbreviations:
BMI: Body mass index; CG: Cockcroft Gault; CKD: Chronic kidney disease; CKD-Epi: Chronic kidney disease -epidemiology consortium equation; eGFR: Estimated glomerular filtration rate; ESRD: End-stage renal disease; GFR: Glomerular filtration rate; MDRD: Modification of diet in renal disease; MEPI-CVD: Medical education partnership initiative on cardiovascular diseases; NCDs: Non communicable diseases; PCA: Principle component analysis; SES: Socio-economic Score; SSA: Sub-Saharan Africa; UNCST: Uganda National Council for Science and Technology (UNCST).
Acknowledgements
We appreciate all the participants (Robert Kalyesubula1,2,6*, Joaniter I. Nankabirwa1, Isaac Ssinabulya1,3, Trishul Siddharthan4, James Kayima1,3, Jane Nakibuuka2, Robert A. Salata5, Charles Mondo2, Moses R. Kamya1 and Donald Hricik5) who took part in the primary study and the all the workers at the MBN lab who participated in analysis of the samples.